Research has uncovered many of the risk factors associated with this common cancer. By identifying the risk factors, we are closer to finding the cause of breast cancer and also by modifying these risk factors, we can reduce our risk. This is the first strategy to combat breast cancer namely prevention or eradication of the cancer. However, this objective is difficult to achieve as some of the risk factors cannot be modified e.g. family history, or lifestyle factors such as child bearing. Despite the intensive search for the cause of breast cancer, the exact cause of breast cancer remains unknown. About 50% of our breast cancer patients have no identifiable risk factors.They can be grouped into the following: -
1.
Age & Sex
2.
Family History
3.
Factors Associated with Reproductive History of a Woman
4.
Dietary Risk Factors
5.
Body Weight and Physical Activity
6.
Intake of Hormones
7.
Previous Abnormal Breast Biopsy
1.
Age & Sex
The risk of breast cancer increases with age. It is uncommon in a woman before 40 years old. 70% of all breast cancers are diagnosed in women 40 years of age and older.Breast cancer can also affect the male but the risk is very low compared to the female. However, when a breast cancer is diagnosed in a male it is often at an advanced stage because of the small size of the male breast.
2.
Family History
A woman with this risk factor has a first degree relative (i.e. sister, mother or maternal grandmother) with breast cancer. Her risk is doubled (2X) when compared to a woman without this risk factor. (See side bar on How to Estimate one’s risk from breast cancer?) However, family history is not a significant risk factor as only 10% of breast cancer patients have it. Our recommendation for woman with this risk factor is to start breast screening at an earlier age at approximately 35 years old.This risk factor comes from the inheritance of genes from our parents and ancestors. Genes contain encoded information and are stored in our cells and passed on from generation to generation. The information contained in our genes is needed for the normal function of our cells. When our genes are damaged, cell function become abnormal and a cancer may be formed. We have identified certain genes, which may be responsible for breast cancer. Inheritance of abnormal forms of such genes increases a woman’s chance of getting breast cancer. Two such genes recently identified are BRCA1 and BRCA2 genes and inheritance of abnormal copies of either of such genes increase a woman’s risk by several fold! Such a woman will have a 40 to 60% of developing breast cancer in her lifetime.Tests to detect such abnormal genes are at present difficult and performed mostly in research laboratories. If you are interested in such tests, you should consult your doctor. There are laboratories in Australia and America, which offer this service.There is another way to identify a woman with these abnormal genes (BRCA1 and/or BRCA2). Her family history is more extensive and stronger with the following features:
§
Many relatives developing breast cancer at an early age(< name="Factors">Factors Associated with The Reproductive History of a Woman.
Research has identified certain aspects of a woman’s reproductive history that can increase her risk from breast cancer. These risk factors are:
§
Woman with no children or having the first child late(after 35 years old)
§
Early onset of menses (earlier than 11 years old)
§
Late cessation of menses (later than 55 years old)
These risk factors are associated with an early and prolonged exposure to oestrogen, which is one of the female sex hormone.A woman attempting to modify these risk factors to reduce her risk from breast cancer will find it difficult to do so as it could mean substantial alterations in her lifestyle. There are calls in America to make changes in colleges and the work place to facilitate a woman’s wish to have children early. Another measure that is being considered is to encourage young girls to exercise more, as it is known that physical activity can delay the onset of menses and suppress the secretion of oestrogen. Can breast-feeding alter this exposure of oestrogen and hence reduce a woman’s risk? Yes, but only if the period of breast-feeding is prolonged (e.g > a year).
3.
Dietary Risk Factors
It has been known for a long time that eating too much red meat and animal fat and too little fibre (vegetables & fruits) may increase a woman’s risk of breast cancer. Recent research has failed to prove this conclusively and controversy still surrounds the role of diet as a risk factor. However, Health Authorities such as the National Institute of Health and American Cancer Society recommend limiting intake of saturated animal fats (less than 20% daily fat allowance) and increasing intake of fruits and vegetables (5 servings daily) to reduce our risks from cardiovascular disease and cancer especially breast, colon and prostate cancer.There is less controversy regarding alcohol as a risk factor for breast cancer. Studies have shown that drinking 1 to 2 glasses of alcohol daily can increase a woman’s risk (relative risk 1.5 times)
Other nutrients that have been identified to alter a woman’s risk from breast cancer are:
§
Soy products as in tauhoo, soya bean juice have been shown in studies to reduce a woman’s risk from breast cancer. This may explain why Asian women have a lower risk from breast cancer compared to American women.
§
Omega 3 oil found in fish. Some studies showed that it could reduce a woman’s risk from breast cancer.
§
Other nutrients that have been found to be protective against breast cancer are vitamin A, selenium, vitamin C & E.
4.
Body Weight and Physical Activity
Weight gain especially in postmenopausal women is associated with an increased risk from breast cancer. This can be a combination of high calories and fat intake as well as a lack of exercise. Some Europeans studies have correlated physical activity to the risk of breast cancer. Physical exercise reduces a woman’s risk of breast cancer by lowering her body’s level of oestrogen.A woman should engage in regular physical activities and moderate her calories and fat intake and avoid weight gain. Her weight should not be more than 20% above her ideal weight.
5.
Intake of Hormones
There are 2 periods in a woman’s life that she wants to take oestrogen (± progesterone) supplement:
§
Hormone Replacement Therapy (HRT). A postmenopausal woman has a choice of taking HRT or not. There are PROS and CONS of such a choice and this is not the forum for such a controversial topic. Recent studies from America have shown that long term or current users of HRT have an increased risk of breast cancer (up by 30%) and this risk disappear 3 to 5 years after stopping HRT. A woman should enter into a close discussion with her doctor/doctors before making a decision.
§
Oral Contraceptive Pill (OCP). The Pill is a popular form of birth control and the worry was whether it would increase a woman’s risk of breast cancer. The conclusion from all the many studies performed is that there is little or no increased risk from taking the oral contraceptive pill. Only a small subgroup of woman may be at a higher risk – early and prolonged usage of the OCP (i.e. late teens, more than 10 to 15 years).
6.
Previous Abnormal Breast Biopsy
A woman with a previous breast cancer is at an increased risk of developing cancer of her opposite breast. She should be on regular reviews with her doctor.A few types of breast biopsies are known to have an increased risk of breast cancer, namely: atypical ductal hyperplasia, atypical lobular hyperplasia and lobular carcinoma in-situ. Woman with such breast biopsy reports should have regular screening starting from her mid thirties.
What Can I Do if I Am at High Risk From Breast Cancer?
Doctors can now give a fairly good estimate of a woman’s risk from breast cancer by taking a detailed family, social and medical history.Women who are at high risk from breast cancer will be offered counselling as to how to cope with this knowledge:
i. They are offered breast screening at an earlier age
ii. They are advised on means to alter their lifestyle and diet to reduce their risk.
iii.A recent study from America has shown that tamoxifen, an important anticancer drug can significantly reduce the risk of breast cancer in these women.
iv.These women can consider preventive prophylactic mastectomies as a means to reduce their risk from breast cancer. A recent study from America has shown that high-risk women who underwent bilateral mastectomies have a 90% reduction in their risk. After removal of the breast, it is reconstructed using a woman’s own body tissue or an implant. Because of the psychological consequence and extensive nature of the surgery involved, a woman must consider very carefully this option before deciding on it.
F. How Can We Fight Breast Cancer?What Are The Methods Of Early Detection?
The only effective and proven method to detect breast cancer early is an X-ray of the breasts called Mammogram. Mammogram is able to detect microcalcifications (calcium dots), which is an early sign of non-invasive duct cancer, and also breast cancers that are too small to be detected by clinical examination (less than 1 cm diameter). Other methods such as Breast Self Examination, Clinical Examination, Ultrasound Scan (Breasts) have not been proven to be effective.
Is Mammogram Painful?
A certain amount of compression of the breast is required to obtain a clear image on the mammogram. This may be uncomfortable and painful. However in a survey in UK, only 10% of women said it was painful.
Is Mammogram Harmful?
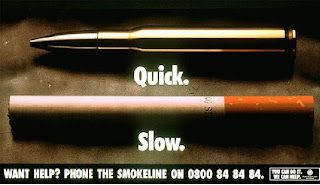
The common belief is that since mammogram is a form of X-ray it is harmful to our body. However the radiation dose from mammograms is quite low and hence the risk to our health remains low. The risk is comparable to smoking 3 cigarettes!
Is There Any Proof That Breast Screening Works?
YES. Studies in US and Europe have shown that regular breast screening in women aged 40 years and above can reduce the risk of death from breast cancer by up to 50%. This translates into lives saved.
Is Breast Screening Effective In All Women?
Studies have shown that Breast Screening is most effective in women 50 to 70 years old. The effectiveness of breast screening for women in her seventies remains unproven.
Where Can I Go For Breast Screening?
Breast Screening is available as part of a general health check in Well Women Clinics found in most government outpatient clinics and Singapore Cancer Society. Breast screening involves a clinical breast examination performed by the doctor followed by a mammogram. Facilities for mammogram and X-rays are available in most hospitals.
The Ministry of Health has just launched a nationwide campaign to screen women above 40 years for breast cancer. The cost of mammogram is heavily subsidized.
What Happens If A Woman’s Mammogram Is Abnormal?
This does not mean that the woman has breast cancer. A large proportion of the abnormalities found on mammogram are not due to cancer. The woman will be recalled by the doctor for further tests such as magnification views of the mammograms and ultrasound scans. Only in a small proportion of women, an abnormality suspicious of cancer is confirmed by these further tests. These women are offered a surgical biopsy to rule out a cancer.
What Is A Surgical Biopsy?
This is a small operation to remove the abnormality in the breast for laboratory examination to rule out a cancer. This operation is usually performed under general anaesthesia as a day surgery procedure.
What Are The Disadvantages of Breast Screening?
-I have mentioned earlier that mammogram is painful to some women and there is a small risk from radiation exposure
-Unfortunately no diagnostic tests including mammogram are 100 percent accurate and some normal women may have mammograms showing an abnormal result. They have to undergo further tests and surgical biopsy to rule out a cancer. This can be costly and inconvenient to these women. Such women may also be subjected to unnecessary mental stress.
-On the other hand, some women with breast cancer may have a normal mammogram i.e. the cancer was missed by the tests. Such women may be falsely assured.
What Are Our Government’s Guidelines For Breast Screening?
40 years and below
Monthly Breast Self Examination
Clinical Breast Examination every 3 years
40 to 49 years
Monthly Breast Self Examination
Clinical Breast Examination yearly
Mammogram yearly
50 years and above
Monthly Breast Self Examination
Clinical Breast Examination yearly
Mammogram every 2 years
H. How Does Breast Cancer Present?
The commonest presentations of a breast cancer in decreasing order of frequency are:
1. Breast lumpq Bloody nipple dischargeq Skin changesq Itchy rash of the nippleq Breast pain
Are all breast lumps cancerous?
The answer is no. In fact 8 out of 10 breast lumps are benign or non cancerous. The type of breast lump depends on the woman’s age.
Twenties
The commonest type of breast lump in this age group is a fibroadenoma. It also known as a breast mouse as it is mobile i.e. it can be moved within the breast. This lump is non cancerous.
Thirties
The commonest type of lump in this age group is known as fibroadenosis or fibrocystic disease. It is often a painful hard area in the outer guardant of the breast and is associated with the female sex hormone, oestrogen. It is non cancerous.
Forties and beyond
Two types of breast lumps are common in older women. One is a breast cyst which is a lump filled with fluid. Breast cyst can be diagnosed by an ultrasound scan and is treated by needle puncture to extract the fluid.
Breast cancer is the other type of breast lump to consider in older women. This lump is usually hard irregular and fixed inside the breast. Changes of skin over the cancer may be seen (thickening, redness depression, skin sore).
I. How Is Breast Cancer Diagnosed?
The doctor depends on three tests to help to diagnose a breast cancer:
-Clinical Examination. Depending on his experience, a doctor can suspect whether a breast lump is cancerous or not by performing a clinical breast examination. Breast lumps or cancers smaller than 1.5cm diameter or situated deep in the breast cannot be detected by clinical palpation. Accuracy of this diagnostic method is approximately 60 to 70%.
-X-ray Mammogram. This is an x-ray examination of the breast and a cancer can appear as an irregular mass, clustered microcalcifications or distortion of the breast tissue. Mammogram can detect breast cancer when it is small and not clinically palpable and hence is very useful in early detection of breast cancer. See section on Breast Screening for more details on this test.
-Breast Ultrasound Scan. This method which uses sound waves to generate an image of the breast is useful in detecting breast lumps in the younger women (less than 35 years) in whom the breast is often lumpy and hence difficult to palpate and whose mammograms are difficult to interpret. Presently ultrasound scan is especially useful to differentiate between a solid lump and a cyst. A breast cancer appears as an irregular tall mass with indistinct margins on the ultrasound scan. The role of breast ultrasound is to complement x-ray mammogram.
Based on these three tests, a doctor is able to suspect whether a lump is present and whether it is cancerous.
Very often, a doctor will recommend a BIOPSY of a breast lump detected by any of the three tests in order to exclude a malignancy. A biopsy is an invasive technique in which some tissue is obtained from the lump for laboratory tests to determine its exact nature.
The common biopsy techniques are:
-Fine Needle Aspiration (FNA). A small needle is introduced into the breast lump to sample it. The aspirate is smeared onto a glass side and analysed in the laboratory. An experienced pathologist is able to tell whether the cells in the aspirate are cancerous after studying them under the microscope. Even though it is simple and easy to perform, FNA is not as accurate as the other biopsy techniques for several reasons (a) inadequate number of cells sampled (b) inexperienced pathologist (c) inability to diagnose a noninvasive breast cancer (which requires a piece of the breast cancer for diagnosis)
-Core Needle Biopsy. The core needle is a slightly bigger needle and is able to obtain slices of a breast lump for analysis. Core needle biopsy is more accurate as it is based on analysis of a piece of the breast lump under the microscope (i.e. histological diagnosis). It can also diagnose noninvasive breast cancer. Automated core needle biopsy systems have been invented in which many slices of a breast lump can be obtained via one small skin puncture.
-Excision Biopsy. A doctor may recommend that the whole breast lump be removed (i.e. excised) for histology. This procedure can be performed under local anaesthesia or more often general anaesthesia. The advantage of excision is that the lump is wholly removed from the woman’s breast.
-Frozen Section. This is a technique to prepare tissue for histological examination quickly (duration 15 to 30 mins). With frozen section, a breast cancer can be diagnosed with the patient under general anaesthesia and the proper cancer operation carried out. This saves the patient having to undergo two hospitalizations, one for the excision biopsy and the other for the cancer surgery.
J. How Is Breast Cancer Classified?
For practical purposes, breast cancer can be classified according to the stage (extent of spread), grade (index of aggressiveness of the cancer cells) and oestrogen receptor status (ER). These information are vital and help to predict survival and determine the treatment.
Staging is determined based on the following:
q
Information regarding the tumour size and invasion of the lymph glands in the armpit based on microscopic examination of the tumour and operated specimen.
q
Diagnostic Imaging Studies to study the extent of spread within the body, which includes chest x-ray, ultrasound scan of liver and bone scan.
Stage
Average Survival (%)
0
Non invasive cancer
90
1
Small invasive cancer
75
2
Invasive cancer > 2 cm with lymph gland invasion
60
3
Large invasive cancer > 5cm with invasion of skin
50
4
Widespread or metastatic cancer
50
Grade is determined by examining the cancer cells under the microscope and labeling the cancer cells as grade 1 (well differentiated), least aggressive; grade 2 (moderately differentiated), moderately aggressive and grade 3 (poorly differentiated), most aggressive.
Estrogen receptors are markers found on the surface of breast cancer cells and their presence is determined by tests on the breast cancer. If present, the breast cancer is labeled estrogen receptor positive (ER+) and if absent; the breast cancer is labeled estrogen receptor negative (ER-). This has an important bearing on determining the type of systemic treatment for the patient (see treatment).
K. How Do We Treat Breast Cancer?
Broadly speaking, treatment consists of two parts:
Locoregional Treatment which is the use of Surgery together with Radiotherapy to eliminate the cancer from the breast and armpit lymph nodes (also called axillary lymph nodes)
Systemic Treatment which is the use of Chemotherapy or Hormonal drugs e.g. tamoxifen to eliminate cancer cells in the body. Modern research has shown that clumps of cancer cells called micrometastases may be circulating in the body of a woman with breast cancer.
L. What Does Locoregional Treatment Consist Of?
Local control of the cancer. The two techniques are Mastectomy, which is the removal of the whole breast including the nipple or Lumpectomy, which is also known as Wide Excision. The newer technique is Wide Excision, which is removal of the tumour with a margin of normal breast tissue. The rest of the breast is untouched to maintain good cosmesis.
Axillary or Armpit Surgery
Is Wide Excision a safe option compared to Mastectomy?
After Wide Excision, Radiotherapy is given to the breast for 6 weeks. Research has shown that Wide Excision plus Radiotherapy is a safe option as it also has a low recurrence rate.
Which patients are suitable for Wide Excision plus Radiotherapy?
Tumours less than 2 to 3 cm diameterq Breast of a suitable sizeq Tumour situated away from the nipple
Which patients are not suitable for Wide Excision plus Radiotherapy?
Young women (less than 30 years old) have a high recurrence rate after this procedure.
Women with connective tissue disease are not suitable for radiotherapy
Pregnant women
2 or more tumours within the same breast
Why is Axillary Surgery required?
Axillary Surgery is required to remove lymph glands (called nodes) for diagnostic and therapeutic purposes. Knowing whether the lymph glands are infiltrated by cancer is important in determining the stage of the cancer. Removal of the lymph nodes also prevents recurrence of the cancer in the axilla.
In this operation called Axillary Clearance or Dissection, the surgeon removes all or most of the lymph nodes in the axilla. Some patients may after Axillary Dissection suffer from temporary shoulder stiffness and arm swelling (lymphoedema).
What is sentinel lymph node biopsy (SLN biopsy)?
Recent research has shown that 1 or 2 lymph nodes act as gateway to the axilla and if there is cancerous involvement of the axillary lymph nodes, they will be affected first (sentinel lymph nodes).
By identifying these sentinel nodes and biopsying one of them can determine whether the rest of the axillary lymph nodes are involved by the cancer.
Hence if the SLN biopsy is negative, there is no involvement of the axillary nodes and vice versa. Because of the limited extent of the surgery, SLN biopsy has fewer side effects compared to Axillary Dissection.
Is SLN biopsy suitable for all patients?
The SLN biopsy is a treatment option of patients with:
- Small tumours
- Non-palpable nodes in the axilla.
It is not suitable for patients in which the chances of nodal involvement are high e.g. large tumours, palpable nodes. In such patients an Axillary Dissection should be performed.
It is also not suitable for patients in which the chances of nodal involvement are low e.g. non-invasive tumours. In such patients no Axillary surgery is required.
Is SLN biopsy a safe option compared to Axillary Dissection?
This new technique is controversial and being evaluated. It is not recommended for routine use.
Is there any hope of ‘Saving The Breast’ after mastectomy?
Yes. The breast can be reconstructed and there is a new improved technique of breast reconstruction called Skin Sparing Mastectomy (SSM) and Reconstruction.
Points to note in Breast Reconstruction following mastectomy:
Timing of Reconstruction
·
Immediate: The Reconstruction is performed after the Mastectomy at the same operation. A new modified technique of mastectomy in which more skin is preserved, called Skin Sparing Mastectomy is performed and the breast is reconstructed with an artificial implant and a skin flap harvested from the back to cover the hole left after removal of the nipple.
·
Delayed: The Reconstruction is performed at a second operation anytime after treatment for the breast cancer is completed. This is usually one year after the Mastectomy. The breast is reconstructed with either an artificial implant or skin and muscle flap from the abdomen (TRAM flap) or the back (Lat. Dorsi flap).
Is Reconstruction safe? The presence of an artificial implant or a reconstructed breast has not been found to interfere with the detection of local recurrence of the cancer or to increase the risk of local recurrence.
What are the types of Reconstruction? As discussed earlier the breast can be reconstructed using an artificial implant (usually silicon) or a skin-muscle flap from the woman’s body. The implant method is quicker (hence less expensive) but some women object to the presence of a foreign body inside them. There has been a lot of controversy whether a silicon implant can cause long-term side effects and the US Food & Drug Administration (FNA) banned the use of silicon implants for cosmetic purposes at one stage. The flap method is the natural method but it takes much longer (hence more expensive) and there may be some problems at the donor site.
Is Breast Reconstruction popular? Not among Singapore women. Only 10% or less of our local women opt for Reconstruction after Mastectomy in a survey conducted and the reasons were
·
More worried about the cancer and less concerned about cosmesis
·
‘Extra’ surgery involved and the costs
·
The lopsidedness after Mastectomy is less in local women as the Asian breast is smaller.
·
Availability of external implants worn in the bra
What is the role of Radiotherapy?
Radiotherapy is the use of radiation to treat breast cancer. Currently the most important indication for radiotherapy is local treatment of the conserved breast following a Lumpectomy for breast cancer. It is given over a 6-week period with daily outpatient treatment sessions. Side effects are usually tolerable, few and confined mainly to the treatment area. Another indication for RT is for women after Mastectomy in which the risk of local recurrence is high (lymph nodes +, large tumour > 4cm).
M. What Does Systemic Treatment Consist Of?
There are two questions to answer for a woman with breast cancer considering Systemic Treatment:
- Does she need the Systemic Treatment?q Which Systemic Treatment?
Criteria for Systemic Treatment
Based on the information obtained from microscopic analysis of the breast cancer and axillary lymph nodes and results of imaging studies, a woman is divided into the low risk and high-risk groups.
Low risk:
Oestrogen receptor positive
Lymph node negative
Grade 1 (well differentiated) tumour
Tumour size less than 1cm
High risk:
The rest
Women in the low risk group are offered tamoxifen or none while women in the high-risk group are offered systemic treatment.
Type of Systemic Treatment
There are 3 main forms of Systemic Treatment:
(1)
Cytotoxic Chemotherapy (2)
Hormonal Manipulation (3)
Ovarian Ablation
Cytotoxic Chemotherapy?
This is the administration of toxic drugs usually into the veins (intravenous). Research has identified these drugs as effective in killing cancer cells, at the same time they are toxic to our body. Hence they are administered at controlled dosage over a period of time to limit their toxicity and at the same time achieve their target of eliminating cancer cells.
There are 3 main regimes, each a combination of cytotoxic drugs and the doctor will select which regime is most suitable for the patient. The drugs are then administered at 3 weekly intervals over 4 to 6 months. These regimes are
·
CMF (cyclophosophamide, methotrexate and 5-florouracil)
·
AC (Adriamycin, cyclophosophamide)
·
Taxol based regime
What are the side effects?
Most patients are concerned about the side effects of cytotoxic chemotherapy and it is important to answer a few key questions.
Can cytotoxic chemotherapy kill? Fortunately death resulting from chemotherapy is very uncommon with an incidence of 0.9% reported from one large chemotherapy study. Deaths are caused by overwhelming infection or formation of blood clots in the veins (thromboembolism) and occur in very sick patients.
What is the immediate side effects and how to cope with them?
Even though these acute side effects can be severe, they are usually tolerable and temporary.
List of immediate side effects following chemotherapy:
- Low total white cell count (Less than 2000/ mm3)q Feverq Infectionq Nauseaq Diarrheaq Hair lossq Platelets count (Less than 50,000/ mm3)q Thromboembolismq Cystitisq Weight gain (More than 10%)
Women on chemotherapy can seek advice on how to cope with these side effects from various sources:
- Reading materialsq Doctors and breast care nursesq Support groups
What about long term side effects?
3 major long-term side effects associated with chemotherapy have been identified:
-Premature Menopause. A woman in her forties has a 50% of premature menopause if she undergoes chemotherapy. The effects of menopause is more severe in a younger woman and varies from hot flushes, palpitations, dry skin to more debilitating conditions such as osteoporosis and increased risk from cardiovascular disease. Fortunately a lot can be done to alleviate these effects.
-Cardiac Toxicity. Adriamycin (alias Doxorubicin) is a commonly used drug in chemotherapy, which unfortunately has an effect on the heart, which could lead to heart failure. The incidence of this side effect is low (less than 5%) and can be decreased by several measures:
§
Assessment of cardiac function in women receiving adriamycin based chemotherapy
§
Limiting the dose administered (cumulative dose of less than 300mg/m2)
§
Method of administration
Risk of a second cancer. A few cases of chemotherapy-induced leukemia (cancer of the white blood cells) have been recorded. Fortunately this serious side effect is rare in long-term studies of patients after chemotherapy.
Hormonal Manipulation
This term refers to measures to alter or stop the secretion of estrogen in the woman’s body in order to treat the breast cancer. These measures are:
Tamoxifen. This is a well-known drug that has been used to treat breast cancer for the last 20 years. It is given orally once daily (20mg) and is well tolerated with little side effects. It is effective for the following categories of women:
§
Women at high risk of breast cancer as a preventive drug.
§
Women whose breast cancer is oestrogen receptor positive (ER+) and is at low risk of recurrence, tamoxifen is given as the sole systemic drug.
§
Women whose breast cancer is ER+ and at high risk of recurrence. Hence tamoxipfen is combined with chemotherapy or other measures of hormonal manipulation. (See table for further details)
Ovarian Ablation
This refers to methods to stop the secretion of oestrogen in a woman’s body in order to reduce the stimulation of cancer cells and hence reduce the chance of cancer recurrence. This method applies only to premenopausal women and lead to premature menopause. Ovarian ablation can be achieved by surgical and non surgical methods:
Surgical Oophorectomy. Surgery is required and is permanent. Seldom used nowadays.
Radiation Castration. Radiotherapy given to the patients over a 2 weeks period can “dry up” the ovaries, and stop the secretion of oestrogen permanently. It is a quick and relatively painless method
Ovarian suppression. Secretion of oestrogen by the ovaries is under the control of a master gland (pituitary gland) situated in the brain. Drugs known as GnRHagonist or Groserelin can alter this control mechanism leading to temporary suppression of oestrogen secretion. Ovarian function usually recovers once the drug is stopped. This drug is usually administered via a subcutaneous injection once a month or once in 3 months. This is a relatively expensive method.
Research has shown that ovarian ablation is as effective as chemotherapy in the systemic treatment of women with breast cancer. For women at high risk from cancer recurrence and whose cancer is ER+, ovarian ablation can be an alternative to chemotherapy.
Chart for Systemic Treatment of Breast Cancer
ER +
ER -
Pre menopausal
Post menopausal
Pre menopausal
Post menopausal
Low Risk(E+, LN-, O, G1, T1 tumour size <1cm) er=" Estrogen" tam=" Tamoxifen," chemorx=" Chemotherapy" name="N">N. Rehabilitation After Breast Cancer Treatment
After breast cancer treatment, a woman can be exhausted both mentally and physically. Foremost in her mind would be what is my prognosis (chance of survival). She would also be worried about her recovery from her surgery and chemotherapy and whether she is fit to resume her role as a mother, housewife or worker. Physically she would be exhausted from the effects of surgery, radiotherapy and chemotherapy treatment.
Mental Rehabilitation
A woman should be fully aware of her prognosis i.e. chance of survival. E.g. a stage I breast cancer patient has a 80% chance of surviving 5 years compared to a 60% chance for a stage II breast cancer. (It is important to note that a woman without breast cancer and of the same age does not have a 100% chance either). Knowing her prognosis will calm a woman and allow her to ‘pickup the pieces’ and carry on her life and assume her place in home, workplace and society.
She should not miss her medical reviews with her doctors. This will enable any recurrence to be detected earlier and treated promptly. The follow up schedule is usually 3 to 4 monthly first 2 years, 6 monthly third to fifth year and annually thereafter. Blood and diagnostic imaging tests are performed either 6 monthly or annually.
Her spouse, children, family and friends should be involved in her rehabilitation. We live in communities and encouragement and help from others will enable a woman to heal faster and recover stronger from her disease and treatment.
She should consider joining support groups to listen to how other women cope with their disease and to find mutual support (see support groups for breast cancer for list of such groups in Singapore)
She should consider changing her lifestyle to improve her health and reduce her chance of recurrence. This would include changing her diet. She should increase intake of fluids, vegetables, fruits, nuts, soya products and cut down on salt, saturated fats, red meat and roasted meat. She should do more exercise e.g. 30mins of brisk walking, jogging or swimming 3 times per week. Low fat and meat diet and physical activity are both associated with lower risk of breast cancer. She should take time off to relax and reduce the level of stress in her life. This is a difficult factor to quantify and has not been proven to prolong the survival of breast cancer patients.
Physical Rehabilitation
As with any major surgery, women after breast cancer operation usually feel weak physically and may take up to 6 to 8 weeks to fully recover their strength, vitality and health.
Surgical wounds on the breast and armpit usually heal within 2 weeks. Pain slowly subsides.
Shoulder stiffness on the side of surgery is due to axillary surgery to remove the lymph glands. With daily graduated exercises most women can overcome this stiffness and regain back full range of movement within a few weeks.
Lopsidedness due to the loss of a breast can be overcome by wearing an external prosthesis in the bra. In the first few months when the wound is still tender, a prosthesis made up of cloth with cotton wool is used. Later on a permanent silicon prosthesis made in the shape of a breast is used
Lymphoedema or swelling of the arm on the side of surgery. This usually starts off as a swelling on the back of the hand and forearm. If neglected the swelling gets bigger and spreads up into the upper arm. It also becomes permanent and is unsightly.
The cause of the swelling is due to accumulation of lymphatic fluid in the arm. One reason would be a recurrence of the cancer in the armpit blocking the lymphatic drainage. This is uncommon. The more common reason is that lymphatic drainage is affected as a result of removal of the lymph nodes. Thus with overuse of the arm, lymphatic fluid can accumulate leading to a swollen arm.
Fortunately the incidence of arm swelling is low, less than 5%. It can be prevented by simple measures, which include
- Avoid over-using the armq Avoid impeding the lymphatic drainage e.g. tight clothingq Avoid any procedures e.g. blood takingq Avoid infection of the armq Encourage lymphatic drainage by exercises daily or by wearing compression stockings
The patient should discuss with her doctor in detail ways to avoid arm swelling and also to seek her doctor’s help quickly if she notices any arm swelling.